Thyroid Cancer and I-131 Therapy: Myths, Preparation, and Post-Treatment Care
🩺 Introduction: A Proven Therapy for Thyroid Cancer
When diagnosed early, thyroid cancer is one of the most treatable cancers today — and Radioiodine (I-131) Therapy remains a cornerstone of that success.
At RNM Centre for Nuclear Medicine & Molecular Imaging, Rohtak, our team specializes in safe, effective, and personalized radioiodine treatments for thyroid cancer patients, guided by international best practices and decades of clinical success.
Despite its proven efficacy, many patients still feel anxious due to myths about radiation and therapy isolation. This blog aims to explain the science, safety, and care involved in I-131 therapy — empowering patients with clarity and confidence.
⚛️ Understanding I-131 Therapy
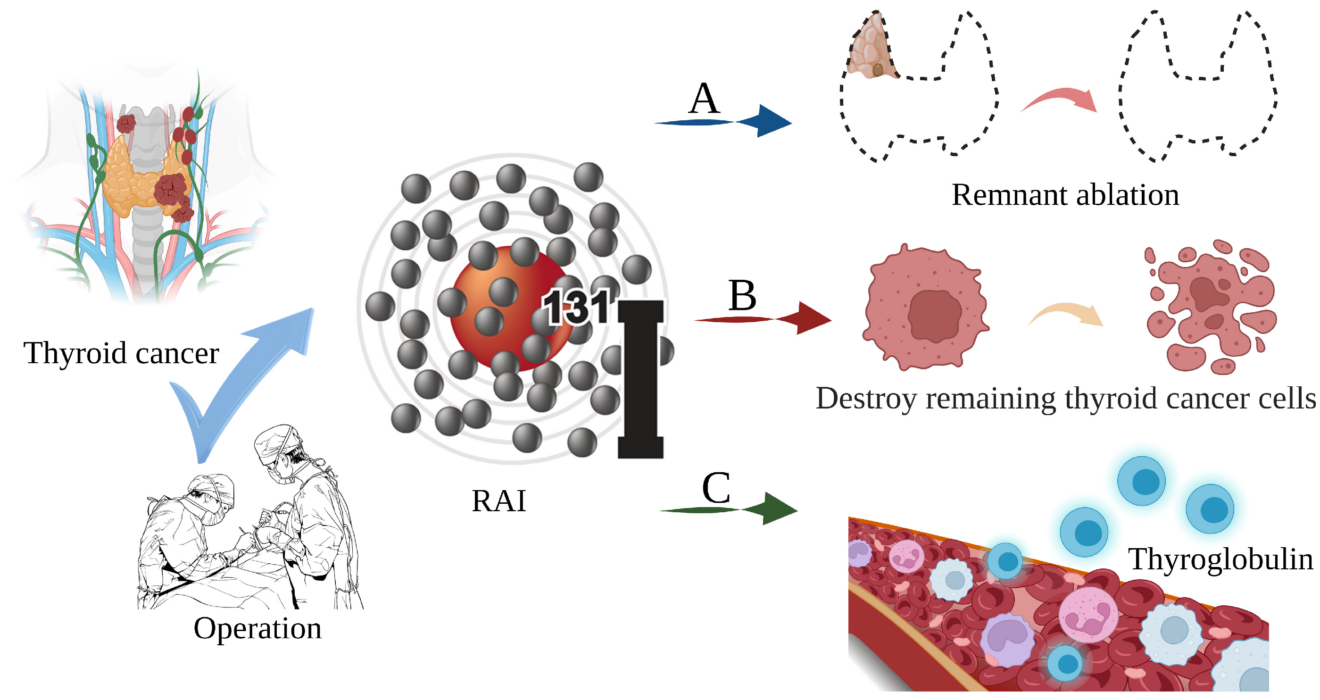
Iodine-131 (I-131) is a radioactive isotope of iodine that selectively targets thyroid cells — both normal and cancerous — due to their natural ability to absorb iodine from the bloodstream.
After a thyroidectomy (surgical removal of the thyroid gland), small amounts of thyroid tissue or microscopic cancer cells may remain. I-131 therapy is administered to destroy these residual cells and reduce the risk of recurrence — without affecting other organs.
💡 How the Therapy Works
- Eligibility Assessment
The nuclear medicine physician evaluates surgical reports, thyroglobulin levels, and diagnostic scans to determine if I-131 is needed. - Preparation Phase
- Low Iodine Diet: Patients follow a low-iodine diet for 1–2 weeks before therapy to enhance uptake.
- Thyroid Hormone Withdrawal or Recombinant TSH Injection: To elevate TSH levels, improving iodine absorption by any remaining thyroid cells.
- Low Iodine Diet: Patients follow a low-iodine diet for 1–2 weeks before therapy to enhance uptake.
- Administration of I-131
The therapy is given orally — as a capsule or liquid — in a controlled hospital setting. - Targeted Action
The radioactive iodine travels through the bloodstream, accumulates in thyroid tissue, and emits beta radiation that destroys residual cancer cells. - Post-Therapy Imaging
A whole-body scan is done 3–7 days later to confirm the iodine distribution and identify any metastases.
🌟 Common Myths vs. Facts
| Myth | Fact |
| “I-131 therapy exposes others to harmful radiation for months.” | False. Radiation exposure drops rapidly, and simple precautions are enough to protect family members. |
| “I’ll lose my voice or ability to speak.” | Untrue. The treatment does not affect vocal cords or speech. |
| “This therapy is painful or invasive.” | Completely false. It’s a simple, painless oral therapy. |
| “I-131 causes infertility.” | No. With proper dosage and medical guidance, fertility and hormone levels remain unaffected. |
| “Radiation remains in the body forever.” | Incorrect. Most radioiodine is eliminated naturally through urine within a few days. |
🧩 Post-Treatment Care and Safety Guidelines
After therapy, patients are typically advised to stay in a radiation-isolated ward for 1–2 days.
Once radiation levels fall below permissible limits, they can safely return home. To ensure safety:
💧 For the First Few Days:
- Drink plenty of fluids to help flush out the isotope.
- Use separate utensils and towels.
- Maintain distance (especially from children and pregnant women) for 5–7 days.
- Follow hygiene precautions when using the toilet (flush twice).
- Sleep separately for a short period.
All these are temporary measures, and radiation exposure to others remains minimal.
🧠 Who Benefits Most from I-131 Therapy
- Papillary and Follicular Thyroid Cancer (Differentiated Thyroid Cancers)
After surgery, I-131 helps eradicate residual disease and prevent recurrence. - Thyroid Cancer with Lymph Node or Distant Spread
It can target and treat metastatic disease, improving survival outcomes. - Thyrotoxicosis (Overactive Thyroid)
In select benign cases like Graves’ disease, lower doses of I-131 can normalize thyroid function safely.
🔬 Follow-Up and Monitoring
- Thyroglobulin Testing: Monitors for any recurrence or metastasis.
- Neck Ultrasound & Diagnostic Scans: Track long-term response.
- Thyroid Hormone Replacement Therapy: Lifelong hormone replacement ensures normal metabolism post-treatment.
RNM Rohtak provides complete care — from pre-therapy counseling to follow-up imaging and hormone management — under one roof.
🚀 Why Choose RNM Rohtak
At RNM Rohtak, all I-131 therapies are conducted in AERB-approved isolation wards, ensuring maximum safety for both patients and caregivers.
Our multidisciplinary team of nuclear medicine physicians, endocrinologists, and technologists provides 360° support — combining science, empathy, and international safety standards.
🏥 About RNM Rohtak
RNM Centre for Nuclear Medicine & Molecular Imaging, Rohtak, is one of North India’s most trusted centers for PET-CT, SPECT-CT, and radionuclide therapies, including I-131 thyroid therapy, Lu-177 PSMA, and DOTATATE treatments.
We take pride in making advanced nuclear medicine accessible, affordable, and patient-focused.